Common Gynaecological Problems And Their Treatment
I. Fibroids Uterus
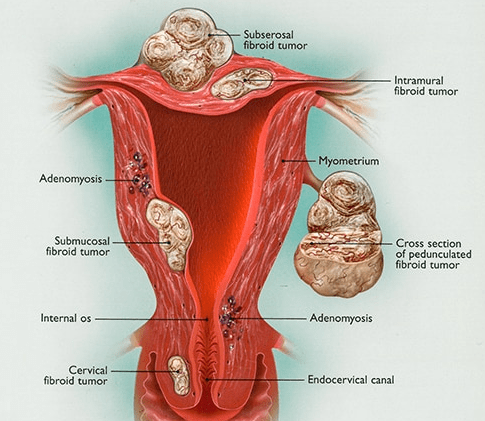
Fibroids are non-cancerous growths that develop in the uterus. A fibroid is made up from muscle fibers and fibrous tissue and is also called Myoma or Leiomyoma. They are usually asymptomatic (i.e. cause no symptoms) and appear in women of reproductive age. It is the most common gynaecological non-cancerous tumor, approximately 20-50% of women will have myomata in their lifetime.
What symptoms can they cause?
Fibroids are usually asymptomatic but they can cause: Heavy menses / Abdominal pain/ Frequent urination / Constipation / Dyspareunia (pain on intercourse) / Fertility problems.
Why do fibroids occur?
While it is not clearly known what causes fibroids, it is believed that each tumor develops from an aberrant muscle cell in the uterus, which multiplies rapidly under the influence of estrogens. There is definitely a genetic component to it, since it is more common in certain racial groups like African Americans and in close relatives.
How are fibroids diagnosed?
Usually during a routine pelvic exam because they are asymptomatic most of the time.
Pelvic ultrasound either transvaginally or transabdominally can identify most of the fibroids and give us accurate information about the size and location of the tumors. MRI is reserved only for multiple complex fibroids or if the consistency of the fibroids is heterogeneous.
What are the complications of Fibriods?
These are as under
- Severe pain or heavy bleeding
- Anemia
- Infertility: This occurs when enlarging fibroids destroy the normal architecture and function of the uterus
- Fibroids in or impinging on the uterine cavity, preventing proper childbirth and causing heavy bleeding.
- Fibroids in the uterine muscle. Larger fibroids can obstruct fallopian tubes, thereby preventing pregnancy, and can also affect normal delivery by preventing delivery of the baby through the vagina. In addition, muscle fibroids can significantly affect fetal growth at larger sizes, and should be removed.
- Urinary tract complications: Fibroids can obstruct the urinary tract, causing severe urinary retention and urinary tract infections, and urinary frequency can also become a serious problem, such as with fatigue from loss of sleep and dysfunction in normal activities of daily living
- Bowel complications: These include severe constipation, bloating, and distension
- Problems at delivery: These include premature birth and Intrauterine Growth Restriction (IUGR)
- Twisting of the fibroids causing severe pain and the need for emergency surgery
What is the treatment for fibroids?
We only suggest intervention when the fibroids cause symptoms or if they might have implications on the patient’s fertility. Watchful waiting is the usual advice for patients with fibroids. The various other procedures are as
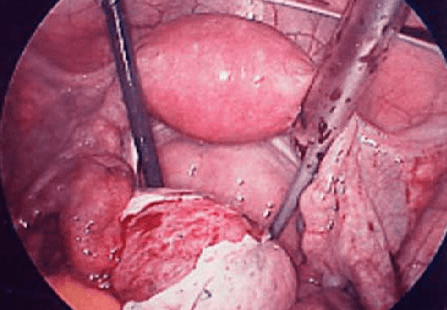
Myomectomy: The surgical removal of the fibroids. This can be done Laparoscopically, Hysteroscopically or via Open Laparotomy, depending on the size , location, number and off course the indication/difficulty of the surgery.
Hysterectomy: The surgical removal of the uterus, including the fibroids. This is usually reserved only for patients that have completed their childbearing and suffer from severe symptoms.
Medical Treatment: Since the growth of the fibroids is estrogen depended, hormonal therapy can reduce the size of the tumors but cannot be used for a long duration of time because it has all the side effects of menopause. It is used for short term control of the growth of the fibroids, most of the times pre- operatively.
What are the chances of cancer arising from a fibroid?
The chances of getting leiomyosarcoma (cancer) when you have a fibroid are extremely low. Most studies calculate the risk in being below 1 in a thousand.
This is the reason why we don’t remove them if they do not cause any problems.
Hysteroscopy
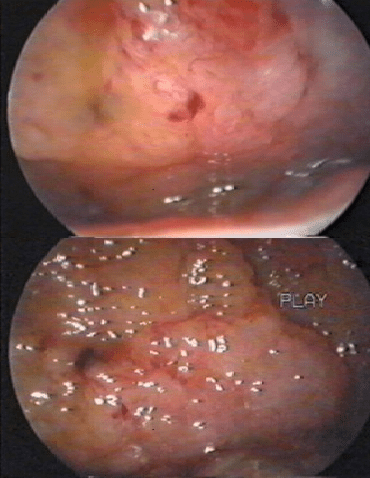
Hysteroscopy can be used for diagnostic purposes to confirm an intrauterine or cervical pathology or in order to treat certain conditions (operative hysteroscopy).
How is Hysteroscopy performed?
Diagnostic hysteroscopy can be performed in the office without anesthesia, especially if a flexible hysteroscope is available.
Operative hysteroscopy is performed under anesthesia, which is usually done in a hospital setting. The cervix is dilated to the appropriate diameter in order to accommodate the hysteroscope. The hysteroscope is a specialized telescopic camera that has 2 small canals. One canal is used to dilate the coaptating endometrial cavity with fluid (normal saline) in order to view the endometrium and the other canal is used in order to pass miniscule instruments. In more complicated hysteroscopic procedures electrosurgical instruments can be used. The procedures usually last a 10-30 minutes.
II. HPV- Cervical Dysplasia
HPV is a virus (Human Papilloma Virus) that affects the skin and the mucosa (moist areas). There are more than 100 types of HPV, and approximately 30 of those affect the genital area.
It is the most common sexually transmitted disease. The chances of being exposed are high.
What causes cervical dysplasia?
A common virus called human papillomavirus (HPV) causes cervical dysplasia. HPV is a sexually transmitted virus, and there are hundreds of strains. Some are low-risk and cause genital warts. Others are high-risk and cause cell changes that can turn into cervical dysplasia and cancer.
What causes cervical dysplasia?
The cells on your cervix can change over time. This means that you can develop cervical dysplasia at almost any age. The presence of cervical dysplasia and/or HPV does not mean you have cervical cancer. However, precancerous cells can become cancerous.
Human papillomavirus (HPV) is the primary cause of cervical dysplasia. There are more than 200 different HPV viruses. About 40 of these affect the genitals. The viruses are spread through sexual contact. Most viruses are low-risk for cancer. About 12 are high-risk. High-risk HPV types 16 and 18 cause about 70 percent of cervical cancer cases. There are several factors that can increase your risk of cervical dysplasia:
Becoming sexually active before age 18, Having a high number of sexual partners, Having illnesses or using medicines that lower your immune system, Smoking or chewing tobacco
Not using condoms (while condoms help prevent HPV, they do not fully protect you), Giving birth before age 16.
How can we diagnose Cervical Dysplasia?
Cervical dysplasia is typically detected during a routine pap test. For this test, doctor swabs cervix to collect a sample of cells. This is generally not painful. The cells are then sent to a lab. It can take up to 3 weeks for the lab to process the test. Inconclusive results do not indicate cervical dysplasia. Patient could have a simple infection in your cervix or vagina. So doctor may order a repeat pap test. Further action or diagnoses will depend on your age and medical history. An abnormal result is known as cervical dysplasia. It is called a squamous intraepithelial lesion (SIL). On the pap test, the precancerous cells may be classified as:
- Low-grade SIL (LSIL), indicating mild abnormality
- High-grade SIL (HSIL), indicating moderate to severe abnormality
- Atypical glandular or squamous cells
Additional testing is needed to see if the cell changes are mild, moderate, or severe. A colposcopy is an in-office procedure that gives your doctor a closer look at your cervix. He or she may gather a larger sample of abnormal tissue, or cells, to biopsy. These biopsies are small and don’t cause much discomfort.
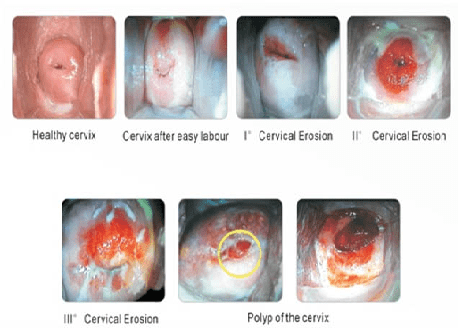
Colposcopy: A way of looking at the cervix and the vagina trough a special magnifying device called colposcope. Special stains are used to highlight any abnormal areas. If a suspicious area is identified then a small sample of tissue (biopsy) may be removed in order to confirm the diagnosis and quantify the extent of the problem. Then you can plan the appropriate therapy if needed. Colposcopy is done usually after an abnormal pap test in order to identify a lesion of HPV infection or cervicitis or a polyp.
Biopsy: A biopsy is the removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make a definite diagnosis. A pathologist then analyzes the sample(s).
What does the HPV cause?
- Genital warts: or else condylomata accuminata are external skin growths of whitish discoloration in the genital region that can be single or accumulate in “cauliflower” like structures.
- Cervical dysplasia: is an atypical appearance of the cells lining the cervix and if it progresses it can lead to cervical cancer in several years.
How can I prevent HPV infection?
HPV is transmitted by sexual intercourse or skin to skin contact of the genital areas. Condom use decreases significantly the chances of transmission. The HPV vaccine gives immunity towards most of the HPV infections and is recommended for administration by most countries before commencing sexual intercourse. It has been shown that women with multiple sexual partners have higher chance of getting an HPV infection.
How much protection does the HPV vaccine offer?
The HPV vaccine offers more than 70% protection for cervical cancer and even greater protection for genital warts.
Is the HPV vaccine safe?
The vaccine is safe and efficient. It has been on the market for more than 10 years and several studies have looked at the side effects proving its safety. The only side affects you can get are, as in most vaccinations, local irritation, pain, fever or rarely an allergic reaction.
How can I be tested for HPV?
Genital warts: can be diagnosed by self-examination if you notice unusual growths or by your gynecologist in the annual exam by inspecting the area.
Cervical dysplasia: is diagnosed with screening tests like the Papanikolaou (Pap) smear on your annual Gyn exam. The frequency of examination depends on your age.
Does HPV cause cancer?
Yes, but luckily very few people from those exposed to HPV will eventually get Cancer.
Low grade atypia in young healthy population reverts to normal on its own in most of the cases (more than 70%).
Can I prevent cervical cancer?
Having had the vaccine and having cervical cancer screening with Pap test can prevent almost all cases of cervical cancer. This way we can identify precancerous lesions, years or even a decade before the actual cancer occurs.
How can I treat HPV infections?
Genital warts: they are usually treated with excision of the lesion and occasionally local destruction with creams/ointments, thermoablation (laser or electrocautery) or cryoablation.
Cervical dysplasias: the depth of the lesion is determined with colposcopic biopsies and then the appropriate therapy is suggested. Which could range from observation or ablation in mild cases and excision of the external portion of the cervix (cone biopsy, LEEP).
III. Ovarian Cysts
Ovarian cysts are fluid filled sacs that originate from the ovary and are usually asymptomatic.
There are two types of cysts:
- Functional cysts: they usually form when the follicle of the menstrual cycle does not rupture. They are benign and short lived. These are the most common ovarian cysts
- Pathological cysts: these are a result of abnormal cell growth or another pathological condition. They are not very common.
How are they diagnosed?
They are usually an incidental finding on a pelvic ultrasound or other imaging modality.
Ultrasound is the preferred method for diagnosis of ovarian cysts, since it can give us a lot of information about the size, position and nature of the cyst. They are usually followed with a repeat ultrasound exam to clarify the nature of the cyst. If a cyst is suspicious for malignancy then cancer markers can be done with a blood test. It is important to stress out that Cancer markers can be high in non-cancerous situations like endometriosis or pelvic inflammation, so it does not necessarily means that you have cancer.
How are they treated?
Most functional cysts do not need treatment because they disappear on their own.
Some pathological cysts might need to be removed. Surgical removal is usually done laparoscopically. In certain situations open laparotomy might be needed. They are usually an incidental finding on a pelvic ultrasound or other imaging modality.
IV. Vaginal Prolapse
Vaginal prolapse is a condition where the bladder, uterus, rectum or small bowel prolapse (fall out of their normal position) into the vagina or sometimes out of the introitus.
What are the types of prolapse?
- Cystocele: when the bladder prolapses, creating a bulge in the anterior vaginal wall.
- Rectocele: when the rectum prolapses, creating a bulge in the posterior vaginal wall.
- Enterocele: when the apex of the vagina drops, containing usually loops of small bowel covered by the vaginal wall.
- Uterine prolapse: when the uterus prolapses in the vaginal canal.
There are four stages of uterine prolapse:
- First degree: the uterus drops in the vaginal canal but not up to the introitus.
- Second degree: the uterus drops all the way to the introitus.
- Third degree: the uterus is visible outside the introitus.
- Fourth degree: the entire uterus in outside the vagina.
What causes vaginal prolapse?
When the supporting muscles and tissues relax or get traumatized. This can happen with age, especially after menopause but can result after child birth because it can traumatize the surrounding tissues. Also sometimes it can happen after hysterectomy because of lack of proper support.
How is vaginal prolapse treated?
There are certain exercises that can help strengthen the supporting muscles of the vagina in initial stages, but in more severe cases surgery can be considered. In patients not fit for surgery pessary can be helpful.
V. Endometriosis
It is a disorder where the tissue that makes up the uterine lining (the lining of the womb) grows outside the uterus.
Causes of endometriosis: there are several different ideas of how and why endometriosis happens. One idea is that when a woman has her period, some of the blood and tissue from her uterus travels out through the fallopian tubes and into the abdominal cavity. This is called retrograde menstruation. Another idea is that some cells in the body outside of the uterus can change to become the same kind of cells that line the uterus. This is a common explanation for endometriosis at unusual sites like the thumb or knee.
Endometriosis Symptoms:
Pain, including pelvic or lower abdominal pain and pain with menses, is the most common symptom of endometriosis. Women may also have pain with intercourse. The symptoms are often “cyclical” meaning that the pain is worse right before or during the period, and then improves. Women may have constant pelvic or lower abdominal pain as well. Other symptoms include subfertility, bowel and bladder symptoms (such as pain with bowel movements, bloating, constipation, blood in the urine, or pain with urination), and possibly abnormal vaginal bleeding.
Diagnosis:
- Laparoscopy: Laparoscopy is considered the primary diagnostic modality for endometriosis. This is an invasive procedure with an overall sensitivity of 97% but with a specificity of only 77%.
- Ultrasonography – Endometriosis can be assessed by either transvaginal ultrasonography or endorectal ultrasonography.
- Magnetic resonance imaging (MRI)
Complications:
Complications of endometriosis include internal scarring, adhesions, pelvic cysts, chocolate cysts of ovaries, ruptured cysts, and bowel and ureter obstruction resulting from pelvic adhesions, endometriosis-associated infertility can be related to scar formation and anatomical distortions due to the endometriosis. Ovarian endometriosis may complicate pregnancy by decidualization, abscess and/or rupture.
Treatment:
While there is no cure for endometriosis, there are two types of interventions; treatment of pain and treatment of endometriosis-associated infertility. Non-steroidal anti-inflammatory medications, like ibuprofen, may help with the pain associated with endometriosis. Some doctors may prescribe medications that affect a woman’s hormones in order to help with endometriosis pain. Some examples are oral contraceptive pills and gonadotropin releasing hormone (GnRH) agonists, the latter of which put women into a “temporary” menopause-like state. Surgery has been shown to improve pain symptoms associated with endometriosis and may also help women become pregnant.
VI. Ectopic Pregnancy
Ectopic pregnancy is the result of a flaw in human reproductive physiology that allows the conceptus to implant and mature outside the endometrial cavity, which ultimately ends in the death of the fetus.
Signs and symptoms:
The classic clinical triad of ectopic pregnancy is as follows: Abdominal pain, Amenorrhea, Vaginal bleeding. Patients may present with other symptoms common to early pregnancy (e.g., nausea, breast fullness). The presence of the following signs suggests a surgical emergency: Abdominal rigidity, involuntary guarding, severe pain abdomen, Evidence of hypovolemic shock (e.g., orthostatic blood pressure changes, tachycardia).
Diagnosis
- Serum β-HCG levels: In a normal pregnancy, the β-HCG level doubles every 48-72 hours until it reaches 10,000-20,000mIU/mL. In ectopic pregnancies, β-HCG levels usually increase less. Mean serum β-HCG levels are lower in ectopic pregnancies than in healthy pregnancies.
- Ultrasonography: Ultrasonography is probably the most important tool for diagnosing an extrauterine pregnancy.
- Transvaginal ultrasonography, or endovaginal ultrasonography, can be used to visualize an intrauterine pregnancy by 24 days post ovulation or 38 days after the last menstrual period (about 1 week earlier than transabdominal ultrasonography).
Management:
Therapeutic options in ectopic pregnancy are as follows:
- Expectant management: Close follow-up and patient compliance are of paramount importance, as tubal rupture may occur despite low and declining serum levels of β-HCG.
- Methotrexate: Methotrexate is the standard medical treatment for unruptured ectopic pregnancy. A single-dose IM injection is the more popular regimen.
- Surgery: Laparoscopy has become the recommended surgical approach in most cases. Laparotomy is usually reserved for patients who are hemodynamically unstable or for patients with cornual ectopic pregnancies
VII. Leucorrhea
Leucorrhea is flow of a whitish, yellowish, or greenish discharge from the vagina of the female that may be normal or that may be a sign of infection. Such discharges may originate from the vagina, ovaries, fallopian tubes, or, most commonly, the cervix. Leucorrhea may occur during pregnancy and is considered normal when the discharge is thin, white, and relatively odourless.
Physiologic Leucorrhea
Physiologic leucorrhea is a normal condition occurring within several months to a year of the onset of menses in adolescent girls and is sometimes present in newborn girls, usually lasting one to two months. However, in many cases, Leucorrhea is a sign of infection, especially when the discharge is yellow or green, has an offensive odour, and is accompanied by irritation, itching, pain, or tissue inflammation.
Abnormal Leucorrhea
Abnormal leucorrhea may be caused by infections with bacteria, yeast, or other microorganisms. For example, many sexually transmitted diseases, which involve the transmission of viruses or bacteria and include diseases such as gonorrhoea and chlamydia, are major causes of leucorrhea. These diseases lead to infection of the cervix, which is indeed one of the most common gynaecological disorders. The infection has a tendency to irritate the mucus glands of the cervix, causing them to secrete an excess of mucous mixed with pus. Leucorrhea is also a sign of vaginitis (inflammation of the vagina), which is often caused by infection with the fungus Candida albicans or by infection with the protozoan parasite Trichomonas vaginalis. Infection with these organisms may give rise to an irritating discharge that is often quite resistant to treatment. A tampon, diaphragm, or other foreign object left too long in the vagina can also cause Leucorrhea. Douching is not recommended, since this practice often disturbs the balance of normal vaginal flora, thereby exacerbating infection. A clinical examination to determine the cause of the discharge is necessary.
This condition can be prevented by following the measures.
- Having a healthy diet.
- Maintaining good personal hygiene.
- Treatment of the underlying infection and typically involves administration of an antimicrobial agent.
Menopausal Problems
A) Post Menopausal Problems
The menopause transition is experienced by 1.5 million women each year and often involves troublesome symptoms, including vasomotor symptoms, vaginal dryness, decreased libido, insomnia, fatigue, and joint pain. Menopause usually starts between the ages of 40 and 58 years in developed countries, where the average age is 51 years. For some, it will occur earlier due to a medical condition or treatment, such as the removal of the ovaries. Around the time of menopause, many females experience physical symptoms such as hot flashes, night sweats, vaginal dryness, and a reduced sex drive. It can also lead to anxiety, changes in mood, and a reduced sex drive. It can last for several years, and there are three stages:
Perimenopause is the transitional time that starts before menopause and includes the 12 months that follow a person’s last period.
Menopause starts either 12 months after the last period or when menstruation has stopped for a clinical reason, such as the removal of the ovaries.
Postmenopause refers to the years after menopause, although it can be difficult to know when menopause finished and postmenopause starts.
Signs and symptoms
Around menopause, various physical and mental changes can occur, causing symptoms. Some of these start before menopause, and some continue after it. The changes involved in perimenopause and menopause include:
- Lower fertility: As a female approaches the end of the reproductive stage, but before menopause begins, estrogen levels start to fall. This reduces the chances of becoming pregnant.
- Irregular menstruation: The first sign that menopause is approaching is usually periods occurring less regularly. They may come more or less frequently than usual, and they may be heavier or lighter. Anyone who has concerns about menstrual changes should see a doctor, as these changes can also indicate pregnancy or some health issues.
- Vaginal dryness and discomfort: Vaginal dryness, itching, and discomfort may start during perimenopause and continue into menopause. A person with any of these symptoms may experience chafing and discomfort during vaginal sex. Also, if the skin breaks, this can increase the risk of infection.
- Atrophic vaginitis, which involves thinning, drying, and inflammation of the vaginal wall, can sometimes occur during menopause. Various moisturizers, lubricants, and medications can relieve vaginal dryness and associated issues.
- Hot flashes: Hot flashes are common around the time of menopause. They cause a person to feel a sudden sensation of heat in the upper body. The sensation may start in the face, neck, or chest and progress upward or downward. A hot flash can also cause: sweating, red patches to form on the skin. Hot flashes usually occur in the first year after menstruation ends, but they can continue for up to 14 years after menopause.
- Sleep disturbances: Sleep problems can arise during menopause, and they may stem from: anxiety, night sweats, an increased need to urinate. Getting plenty of exercise and avoiding heavy meals before bedtime can help with managing these issues, but if they persist, contact a healthcare provider.
- Emotional changes: Depression, anxiety, and low mood are common during menopause. It is not unusual to experience times of irritability and crying spells. While feelings of sadness, irritability, and tiredness are common during menopause, they do not necessarily indicate depression. Treatment: Treatments may include:
- Lifestyle and home remedies: Fortunately, many of the signs and symptoms associated with menopause are temporary. Take these steps to help reduce or prevent their effects:
- Cool hot flashes: Dress in layers, have a cold glass of water or go somewhere cooler. Try to pinpoint what triggers your hot flashes. For many women, triggers may include hot beverages, caffeine, spicy foods, alcohol, stress, hot weather and even a warm room.
- Decrease vaginal discomfort. Use over-the-counter, water-based vaginal lubricants, silicone-based lubricants or moisturizers. Choose products that don’t contain glycerin, which can cause burning or irritation in women who are sensitive to that chemical. Staying sexually active also helps by increasing blood flow to the vagina.
- Get enough sleep. Avoid caffeine, which can make it hard to get to sleep, and avoid drinking too much alcohol, which can interrupt sleep. Exercise during the day, although not right before bedtime. If hot flashes disturb your sleep, you may need to find a way to manage them before you can get adequate rest.
- Practice relaxation techniques. Techniques such as massage and progressive muscle relaxation may help with menopausal symptoms.
- Strengthen your pelvic floor. Pelvic floor muscle exercises, called Kegel exercises, can improve some forms of urinary incontinence.
- Eat a balanced diet. Include a variety of fruits, vegetables and whole grains. Limit saturated fats, oils and sugars. Ask your provider if you need calcium or vitamin D supplements to help meet daily requirements.
- Exercise regularly. Get regular physical activity or exercise on most days to help protect against heart disease, diabetes, osteoporosis and other conditions associated with aging.
Medical Treatment:
- Hormone therapy. Estrogen therapy is the most effective treatment option for relieving menopausal hot flashes. Depending on your personal and family medical history, your doctor may recommend estrogen in the lowest dose and the shortest time frame needed to provide symptom relief for you. If you still have your uterus, you’ll need progestin in addition to estrogen. Estrogen also helps prevent bone loss. Long-term use of hormone therapy may have some cardiovascular and breast cancer risks, but starting hormones around the time of menopause has shown benefits for some women. You and your doctor will discuss the benefits and risks of hormone therapy and whether it’s a safe choice for you.
- Vaginal estrogen. To relieve vaginal dryness, estrogen can be administered directly to the vagina using a vaginal cream, tablet or ring. This treatment releases just a small amount of estrogen, which is absorbed by the vaginal tissues. It can help relieve vaginal dryness, discomfort with intercourse and some urinary symptoms.
- Low-dose antidepressants. Certain antidepressants related to the class of drugs called selective serotonin reuptake inhibitors (SSRIs) may decrease menopausal hot flashes. A low-dose antidepressant for management of hot flashes may be useful for women who can’t take estrogen for health reasons or for women who need an antidepressant for a mood disorder.
- Gabapentin / Pregabalin. These agents are useful in women who can’t use estrogen therapy and in those who also have nighttime hot flashes.
- Medications to prevent or treat osteoporosis. Depending on individual needs, doctors may recommend medication to prevent or treat osteoporosis. Several medications are available that help reduce bone loss and risk of fractures. Your doctor might prescribe vitamin D supplements to help strengthen bones.
B) Urinary Incontinence
It is the involuntary leaking of urine. Incontinence can range from a few drops to complete emptying of the bladder.
What are the types of urinary incontinence?
- Stress urinary incontinence (SUI): leaking of urine when extra abdominal pressure is applied, like in sneezing, coughing, laughing or in certain activities.
- Urge Incontinence: is a sudden onset urge to urinate that is hard to stop. Women with this type of incontinence may leak urine on the way to the bathroom.
- Mixed incontinence: combines symptoms of both.
How is the type of urinary incontinence diagnosed?
- Urine analysis: is always requested because a Urinary infection can mimic incontinence symptoms sometimes.
- Medical history: your gynecologist will ask you several questions about the signs and symptoms of your condition and may have you fill in a bladder diary for several days.
- Physical exam: the doctor will examine you to see if you have pelvic organ prolapse and may ask you to perform some test like “cough test”.
- Urodynamic testing: reserved for the cases where the diagnosis is not clear, it is a specialized test using a urinary catheter and electrodes to collect data about several measurements.
How is urinary incontinence treated?
Depending on the type of incontinence we usually start with lifestyle modifications like decreasing the amount of water intake or performing certain exercises (Kegel) and then proceed to medications, pessaries or surgical correction of the incontinence.